I was invited to attend Fortune’s inaugural Brainstorm Health event in San Diego last week, which was full of fascinating conversations both on and off the stage from the predominantly US based health tech leaders who were in attendance. I wanted to share some of my key take outs, along with a great summary of the event here on the Fortune website.

Messages that really resonated for me were on the potential that AI and VR have to impact on the way healthcare is provided, and the way that data and technology can combine to democratise healthcare knowledge and accessibility, all the while acknowledging the ever present challenges of data capture, storage and sharing.
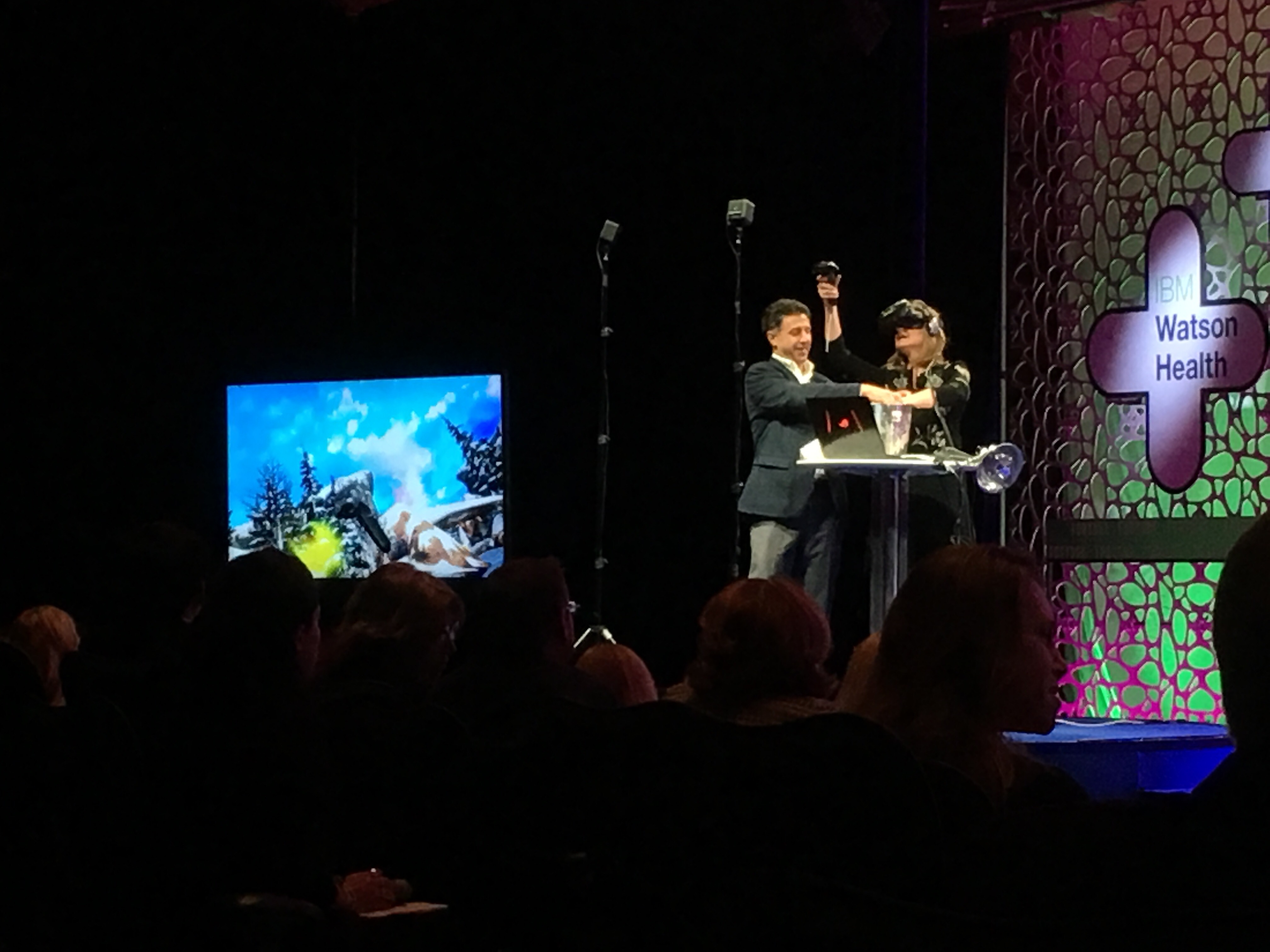
Arianna Huffington happily agreed to play guinea pig to demonstrate the role that DeepStreamVR can play in pain management, comparing the pain experienced by plunging her hand into a bucket of icy water with and without the VR experience. A screen showed us what she was visualising in the headset, and it was obvious that the distraction of trying to hit flying fish with paint balls was taking her mind far away from the discomfort of the icy water! Interestingly research has shown that the benefits of VR in pain management last for hours after the headset is taken off, so the effect is created by something greater than the distraction alone.
We all got to experience the way we can change our brain activity when Deepak Chopra took us through a 20 minute guided meditation exercise after speaking to us on the research that has shown meditation can change gene expression. Meditation has never been something I’ve been able to embrace despite all of the benefits it delivers, my mind wanders and I find myself getting more stressed because I’m so bad at it. This time was different though, I’m not sure whether it was a consequence of having one of the world’s greatest subject matter experts leading the guided meditation, or the fact that I was so exhausted after my second trip to the US in less than a week meant my mind had no energy to fight the process! After getting us to focus initially on our breathing we moved to trying to listen to our heartbeat, before trying to feel the energy of our heartbeat in our fingertips. Much to my amazement I actually could, but I obviously relaxed into it a little more than I should have because I missed the second half after drifting off into a very refreshing snooze. It has left me with a renewed goal of committing to making meditation something I actually do rather than just think I probably should do, so lets see how that goes.
Nicely aligned to the need switch off via tools like meditation was the advice from Arianna Huffington on the importance of sleep and rest. She pointed out that while we’ve created a belief that success and burnout are inextricably linked, its actually fundamentally untrue and we greatly increase our chances of success by giving our bodies and minds the chance to perform at their well rested optimum. Everyone at my table could certainly identify with her suggestion that there was a real disconnect between our obsession with being aware of the battery status of our phones and making sure that we had measures in place to recharge them before they got too low, but few of us gave our own batteries the same consideration.
It’s not a healthcare event however without a significant proportion of the conversations being devoted to the two big dilemma’s our industry faces – how do we shift our focus to prevention rather than treatment, and how do we best utilise the vast quantities of data generated to drive better health outcomes.
Dr Dana Goldman from USC reminded us that health by necessity used to be a disease based model, when we needed to focus on preventing and treating diseases with a very high risk of mortality like smallpox and polio. Now with mortality rates from those conditions transformed by vaccination programs, making progress on one disease is likely to result in an increased risk of another, shifting the focus onto prevention strategies. Dr Anthony Atala talked about the fact that health care professionals don’t see patients until they are already in a disease state, with no visibility of their health data until their health is already compromised. Despite the richness and depth of the data that we do have about patients, it’s the data that we don’t currently have visibility of that is required for prevention strategies to be designed and implemented.
There were lots of conversations about and demonstrations of devices that can help to close this knowledge gap, but with conference co-chair Clifton Leaf telling us that right now less than 1% of data generated by healthcare systems is analysed, adding in the torrent of available new data without strategies to ensure that it’s collected and collated in an actionable and useful way is going to add to the problem rather than deliver any solutions.
This also created an interesting discussion about the lack of standardisation in what metrics wearables are measuring – for example a step is different across every device, and there have been many illustrations of the vast variation in results achieved when multiple devices are worn simultaneously to record the same activity. This lack of standardization adds to the challenge of getting devices FDA approved, with it suggested companies are currently looking at costs ranging from $10-100M to clinically validate the claims wearables are making.
There’s no question that better utilising data can not only improve outcomes but also provide insights that ensure healthcare spend is managed effectively and appropriately. Dr Vivian Lee illlustrated this perfectly sharing learnings from the University of Utah, where an analysis of hip replacement surgeries revealed a huge variation in the cost of the prosthetics used, but no difference in outcomes between expensive and cheaper devices. What it did reveal though was that the patients who had longer stays and slower recoveries were all operated on later in the day when the physical therapists had gone home, impacting on their ability to get ambulatory on the day of their surgery. Putting on a second shift of therapists was the thing that made the difference in equalising outcomes, not shifting everyone to the more expensive prosthetic devices.
But despite all of the potential, there was still a strong sense of frustration around how little progress was being made on changing the long term problems of information access and analysis. It’s still a challenge for patients to obtain their own health care record, let alone share it with practitioners of their choice, and as Dr Kathy Hudson from the National Institutes of Health said, big data isn’t going to help until we can fix our small data problem. Jonathan Bush, CEO of athenahealth, revealed that athena clinics still receive 8 MILLION faxes a week, highlighting how much work there still is to do in getting data into systems that can then have the power of AI harnessed to them. With so much information still so inaccessible, the disconnect between the potential of what’s possible with AI and the reality of what’s currently achievable is real.
Closing this gap requires big changes in the way we capture, store and share data. It’s all possible using widely available, existing technology, but it requires an appetite and a willingness to take on that change. The exciting thing for me is that I believe both of those exist at Icon Group, and the opportunity that gives us to play a transformational role in the way our patients are able to access information and engage in their care partnership is significant.
Brainstorm Health was a great name for this event. Conversations were robust, with differing views on what the priorities should be and what approaches were best which made for real thought stimulation, and I’m very appreciative of the opportunity to attend and participate..
Thanks for the terrific write-up, Cathie! And thank you, most of all, for carving out so much of your busy schedule to be there. All the best, Cliff
Thanks Cliff, it was a great event and well worth the trip!